omgyno is a social enterprise born out of the challenges we face in healthcare, and designed to empower anyone with a female reproductive system. We know that so many of you out there do not have access to a good gynecologist or sexual health services that provide the attention and information you need. We believe that education, human-centered design, technology, advanced diagnostics labs, progressive doctors, and an environment of safe and progressive care can be a vital solution to redesigning our experience with the most intimate part of our bodies.
omgyno offers its community the tools to take control of their bodies and prioritize their health. With lab partners, we have developed carefully designed home test kits for self-sampling, so that anyone can get a test at any time without booking appointments or extra costs. Our team of selected healthcare professionals provide timely expert medical advice and open-mindedness by putting your needs first via telemedicine, so you can receive professional virtual consultation in a safe and private space, wherever you are. Our Shop offers a variety of eco-friendly hygiene products that can provide that extra well-being factor you deserve.
We know that menstrual, sexual, and reproductive health depends on a holistic approach to both physical and mental aspects, so omguide keeps us all informed on ways to ensure that we achieve that goal, for life.
Functioning felt impossible. We kept asking ourselves how we could possibly continue our work when everything around us seemed so fragile.
Due to limited resources, many SRHR responses had to be selective at the time. Yet when a woman in need stands before you, telling her that her care is conditional feels like denying her dignity.
One day, our Instagram page pinged with a message from a woman we’ll call “D,” who had opened a shelter in Hazmieh, and received over 200 migrant domestic workers mostly from Sierra Leone. She asked if we had a mobile clinic. We immediately had one of those ideas that makes everyone roll their eyes—and then roll up their sleeves. “Hold on,” we said. “We can do so much better.”
It sounded nearly impossible. The timeline was tight, the logistics demanding, and the stakes high. But the thing about our team is that when you say “no,” someone always asks, “why not?”
For the next two weeks, we lived on adrenaline. Dimagi offered us a free subscription to CommCare, a HIPAA-compliant platform built for humanitarian field work. Meedan offered to financially support our intervention. Dr. Sarab El Samad helped us design a simple triage system that anyone could use, even without medical training. Doreen and Rosa built the algorithm on CommCare, linking every step of the process, from registration to teleconsultation, and refined it by day and by night. And the rest of the team handled logistics: sourcing kits, coordinating with the lab, printing multilingual instructions, and running an online donation campaign. We barely slept, argued plenty, but kept moving. There wasn’t time for hesitation, only for making it happen.
Our Two Days in Hazmieh
We arrived at the shelter unsure of what to expect. The atmosphere was tense, but there was a quiet sense of purpose among everyone there. We had community health workers (CHWs) ready to help, though we’d never met before.
Day One was about training. We guided the CHWs on how to use CommCare, conduct the triage, and flag anyone needing immediate intervention or follow-up. By the end of the day, every woman in the shelter was registered on the platform, and the CHWs were confidently navigating a system they had just learned.
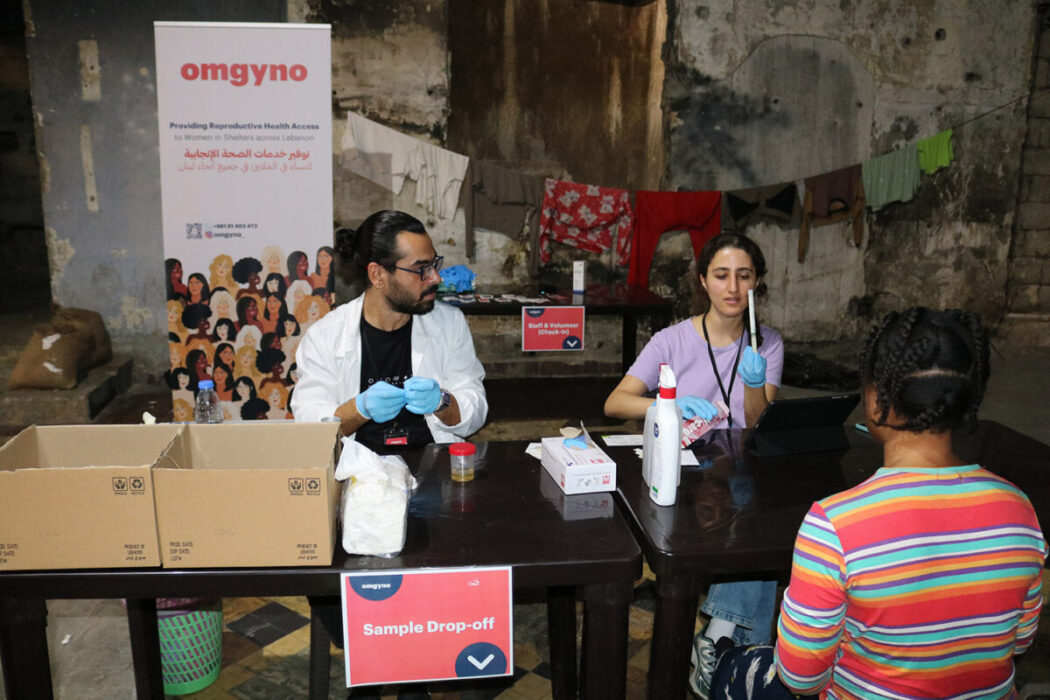
Day Two was when it all came together. We turned part of the shelter into a small clinic with three stations: registration, test pickup and instructions, and sample drop-off.
Those who needed follow-up met Dr. Sarab via Zoom from France.
In a quiet corner of the shelter, they spoke to a doctor abroad while bombs echoed in the distance. It was a brief moment of calm within chaos, a quiet reminder of why we do this work.
What moved me most was witnessing our CHWs, a group of strangers who didn’t know us or each other, come together with commitment, and coordinate effortlessly to make this work. It just seemed like everyone directly found their rhythm.
And then came the women of the shelter. We had assumed they might struggle with self-sampling, but we were wrong. They followed every step with focus and confidence. Out of more than a hundred participants, only one needed help; the rest did it perfectly on their first try. It was us who learned that day to trust them, to trust their ability to take charge of their own health.
Of course, not everything went smoothly. We had some technical issues, a few dropped connections, but our team in Greece was always on call. Part of it was messy and stressful, but it worked. When the results came back from the lab and we were finally able to offer treatment and follow-up care; what I felt wasn’t relief, it was a quiet, collective pride.
They spoke of surviving explosions, then finding one another in shelters—cooking, cleaning, and caring together like family. One woman’s voice trembled as she said: “A couple of days ago I was alone, and pregnant, fleeing the bombs. Now, I found myself with so many sisters here.”
Looking back
Looking back, I still find it hard to believe how much we managed to do with so little time and resources. A small team building and implementing a system of care in two weeks in the middle of a war shouldn’t have worked—but it did.
It worked because of the people who refused to simply look away: the women who trusted us and trusted themselves, the CHWs who showed up without hesitation, the partners who offered their unconditional support, and a team that held everything together when things got hard. It wasn’t perfect, but it was real, and it definitely reminded us that even in the most uncertain times, dignified care can always find a way through.